Physiotherapy for Sever’s Disease
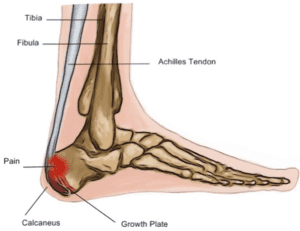
What is Sever’s Disease? Sever’s disease is a condition that causes pain in the heel of children and adolescents. While it can be quite painful,
Alicia Leahy
What is Sever’s Disease? Sever’s disease is a condition that causes pain in the heel of children and adolescents. While it can be quite painful,
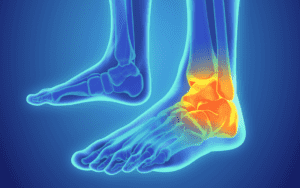
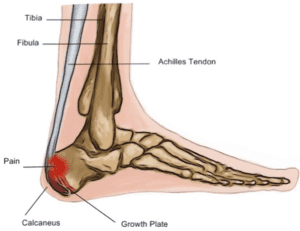
Ankle sprains are one of the most common lower limb injuries in sport, in particular “lateral” ankle sprains which involve the outside ligaments of your

The triangular fibrocartilage complex is located on the ulnar side of the wrist (ie. pinky finger side). It contains a central disc and supporting structures
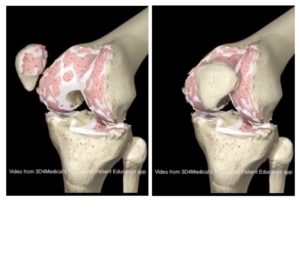
For many decades, the best practice treatments for osteoarthritis were managing pain with medications (pain killers and anti-inflammatory medications) and where pain or disability was severe enough, a referral to a surgeon would be given for
What is a stress fracture? A stress fracture is a small fracture of the bone that is caused by repeated mechanical stress, rather than an

Load management is a popular and sometimes contentious topic amongst health professionals, trainers and sporting institutions. Debates range from how much is too much, how

With the beautiful spring weather just around the corner, it is a popular time to start running or ramping up that fitness regime. Common goals

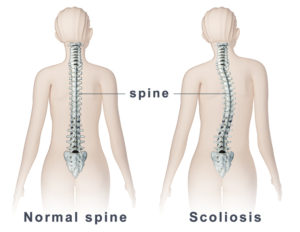
Lower back pain is one of the most common complaints of musculoskeletal pain. Everyone is likely to have known someone or has experienced lower back
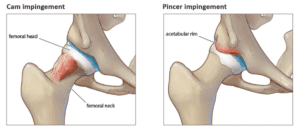
Hip pain is a common issue we see here in the clinic. Patients can complain of a ‘pinching’ when doing things like squats, getting in