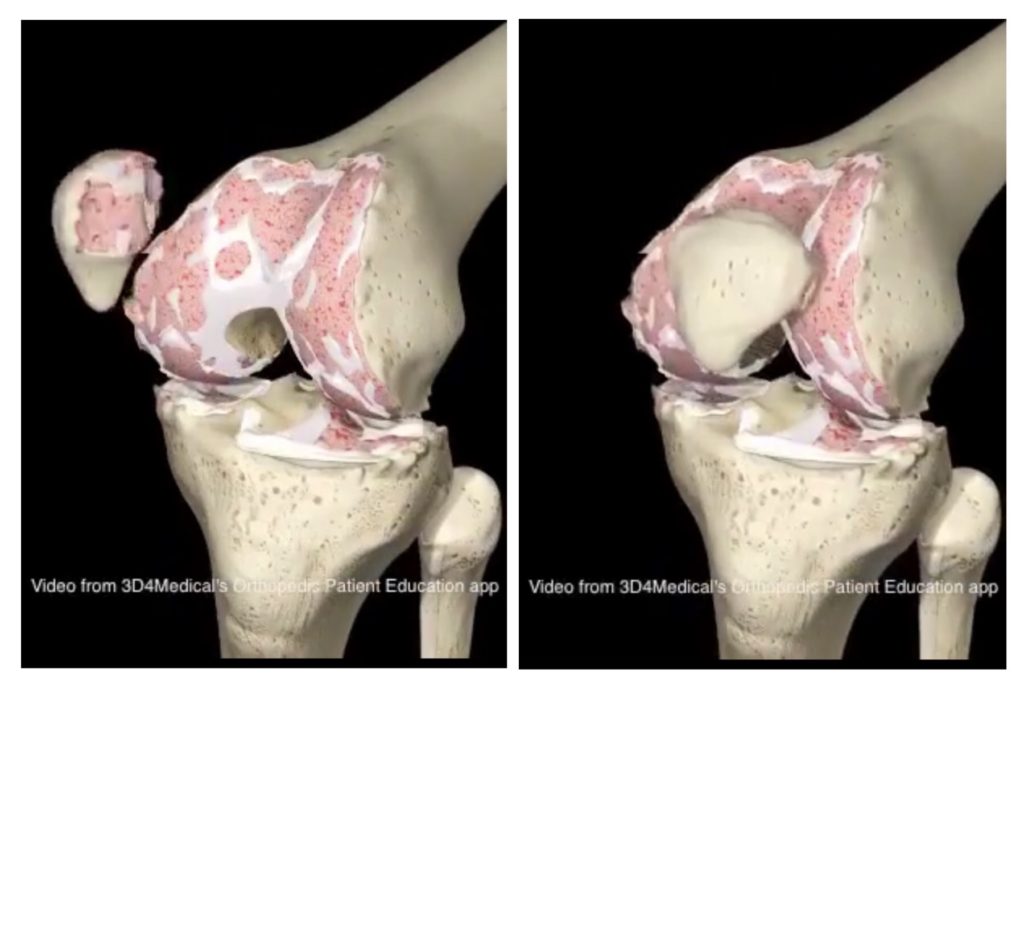
For many decades, the best practice treatments for osteoarthritis were managing pain with medications (pain killers and anti-inflammatory medications) and where pain or disability was severe enough, a referral to a surgeon would be given for a joint “clean out”. This procedure usually involved scraping back bits of bone (osteophytes) and trimming cartilage where it had torn or frayed.
Following countless research studies over the previous 20 years, the usefulness and necessity for surgical clean outs has now decreased for the typical osteoarthritic joint. Whilst there is benefit for surgery in cases that include significant structural deficiency (e.g. Large “bow-legged” and “knock-kneed” knee joints), the idea for arthroscopic clean out of a joint should be regarded as no longer being best practice, nor the best option for the longevity of your joint function.
In relation to seeking scans to confirm the presence of osteoarthritis in the knees, these too have received a change in the Medicare funding arrangements, particularly in the instance of seeking an MRI for confirmation of OA. From 1st November 2018, MRI’s of the knee referred by GP’s are no longer subsidized for people over the age of 50. These come in line with new guidelines for the management of knee and hip osteoarthritis, issued by the Royal Australian College of General Practitioners in July 2018. In this guideline, it states that a typical knee OA diagnosis can be made without requiring further investigations if a person:
- is aged 45 years or older
- has activity-related joint pain
- has morning stiffness that lasts <30 minutes
- has crepitus on active motion
- has bony enlargement
- has no detectable warmth.
Additional features that may be present include:
- deformity – fixed flexion and/or varus (bow legged) and less commonly valgus (knock-knee) for the knee
- instability
- peri-articular or joint-line tenderness
- pain on patellofemoral compression.
Similar to knee OA, hip OA can be diagnosed by clinical features alone. Early physical signs of hip OA include restriction of internal rotation and abduction of the affected hip, with pain occurring at the end of the range of motion.
If you have suffered any of these conditions above, please make a booking with one of our physiotherapists for a thorough examination and implementation of the clinical best practice in managing your arthritis